Blood Glucose Chart
It’s important to talk to a medical provider about blood glucose targets for diabetes. A diabetes management plan helps diabetics or prediabetes searching to control blood glucose levels.
Regular blood glucose tests can help the diabetic to determine how well the diabetes management program, including meal planning, medication (if needed), and exercise is working to maintain blood glucose levels.
National Diabetes Control and Complications Trial (DCCT)
The results of the DCCT show that the better the diabetic maintains his or her glucose levels in the normal range, the better he or she is able to prevent the complications of diabetes, such as nerve damage, kidney disease, or eye disease. Somewhat higher blood glucose levels may be appropriate for diabetics, depending on the management of multiple chronic health conditions and age.
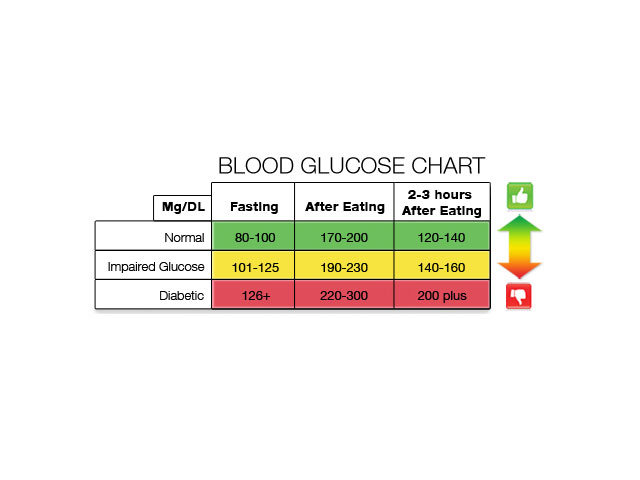
The Blood Glucose Chart below outlines the typical blood glucose for persons managing diabetes or non-diabetics. Use the chart to guide discussions with a doctor or healthcare provider to decide individual blood glucose targets. Develop a blood glucose monitoring program to manage diabetes to protect health.
Blood Glucose Chart
| Blood Glucose Check Time | Plasma Blood Glucose Goal (ranges for non-diabetic people) | Plasma Blood Glucose Goal (ranges for diabetic people) |
| Fasting (before breakfast) | Less than 100 mg/dL | 70 – 130 mg/dL |
| Before meals (lunch, dinner, snack) | Less than 110 mg/dL | 70 – 130 mg/dL |
| Two hours after consuming a meal | Less than 140 mg/dL | Less than 180 mg/dL |
| At bedtime | Less than 120 mg/dL | 90 – 150 mg/dL |
| A1C Level (also called HbA1C, glycosylated hemoglobin A1C, or glycohemoglobin A1C) | Less than 6.0 percent | At or less than 7.0 percent |
What is Diabetes?
Diabetes occurs when the individual’s body can’t correctly use or store glucose. Glucose circulates in the bloodstream.
There are two primary types of diabetes:
- Type 1 diabetes, sometimes called insulin-dependent diabetes, occurs when the diabetic’s body doesn’t produce insulin, a hormone that assists the body in using glucose for energy. Type 1 diabetics take insulin injections each day to survive. Type 1 diabetes typically develops in young people or children, but it may happen at any age.
- Types 2 diabetes, sometimes called adult-onset diabetes, occurs when the individual’s body doesn’t make sufficient insulin or can’t use the insulin the body produces (insulin resistance). Type 2 diabetes most often happens when people are overweight, have a genetic predisposition of diabetes, and or over 40. Today, Type 2 diabetes occurs in younger individuals.
Symptoms of Diabetes
The symptoms of diabetes may include:
- Excessive thirst
- Urinary frequency
- Weight loss
- Irritability
- Unusual hunger
- Blurred vision
- Unexplained extreme fatigue
- Numbness or tingling in feet and hands
- Frequent gum, skin, or bladder infection
- Wounds that won’t heal
Some diabetics have no symptoms at all. The diabetic person may have diabetes for months or years before learning he or she has the disease. The onset of Type 2 diabetes is usually gradual, so many people don’t realize that something isn’t right.
Who Gets Diabetes?
Anyone can get diabetes. Those with close relatives with diabetes have a higher likelihood of developing it. Additional risk factors, such as lack of physical activity, obesity, high blood pressure, or high cholesterol, can promote the development of diabetes.
Older people are more likely to get diabetes:
- Overweight people over the age of 40 have the highest statistical chance of developing diabetes.
- Younger people and children can develop Type 2 diabetes.
- Heritage can place the individual at higher probability of developing diabetes: Native Americans, Asian American/Pacific Islanders, Hispanics, and African Americans are at highest risk of developing diabetes.
- Pregnant women may develop <i>gestational diabetes.</i> This condition places the pregnant woman at risk for developing Type 2 diabetes when she is older.
How is Diabetes Treated?
Diabetics need certain things to stay healthy:
- An eating plan to manage blood glucose
- Physical activity to manage blood glucose
Some people may need insulin or oral medicines to manage their blood glucose and to help their bodies use insulin. People with Type 1 diabetes (and some Type 2 diabetics), need supplemental insulin. Some people with Type 1.5 and Type 2 diabetes take oral medicines to help them produce greater amounts of insulin or to better use the insulin their bodies produce. Other Type 2 diabetics manage the disease with meal planning and sufficient physical exercise.
All people with diabetes should be followed by a diabetologist, endocrinologist, or physical internist:
- He or she should visit a dietician or nurse educator to create a customized meal plan.
- An exercise physiologist can help the diabetic to develop an exercise plan.
- Diabetes complications may include the development of eye problems.
- All diabetics should visit an opthamologist each year.
- Diabetes can cause kidney disease. It may be necessary to consult with a nephrologist to evaluate kidney function.
Although diabetes can cause a range of complications, including heart attacks, vascular disease, strokes, amputation, impotence, kidney failure, nerve damage, or blindness, the good news is that a study showed that keeping blood glucose levels in the normal range (or as close to the average blood glucose range as possible) reduces the risks associated with the development of complications at more than 50 percent.